Corneal Transplant Surgery
Understanding Corneal Transplant Surgery
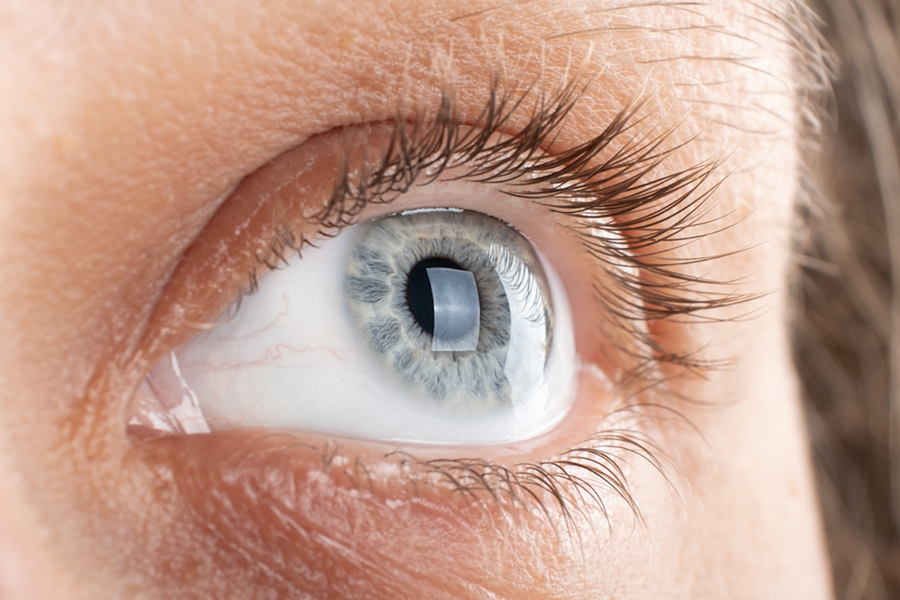
The cornea is the transparent covering of the front of the eye, similar to the crystal of your watch. Swelling or scarring of the cornea blocks passage of light into the eye causing blurred vision. In corneal transplantation surgery we replace the cloudy cornea with a clear one. Corneal transplantation is the most common transplant operation performed today with over 35,000 procedures done annually in this country. With modern technology over 95% of corneas remain clear.
The Procedure: What Happens During Corneal Transplantation
During corneal transplantation we remove a central disc from your cornea and replace it with a cornea donated by an organ donor. There are very strict precautions covering donation of tissue to ensure that there is no transmission of disease through the donated cornea. This includes blood testing for AIDS and hepatitis.
To secure the cornea in place I use extremely fine sutures, finer than a human hair. When I sew the new cornea in place I try to do a perfect job, however due to the shape of the cornea, or your healing pattern, there may be astigmatism. This occurs when the cornea is shaped like a football, rather than a basketball. During the visits to the office post-operatively we measure the astigmatism and try to reduce it by selectively removing sutures. This is done using drops only. It is easier to remove the sutures than to place them! After a period of healing ranging from 3 to 12 months, the cornea has stabilized sufficiently to prescribe glasses, or rarely, a contact lens, to obtain the best vision. Not all sutures need to be removed so some may stay in place indefinitely.
Post-Surgery Care and Recovery
Although corneal transplantation is very successful, complications can occur. In extremely rare cases vision can be lost completely in the operative eye if an infection or hemorrhage develops.
The most common obstacle to good vision after corneal transplantation is swelling of the retina (macular edema) which may be existing prior to surgery or may develop after surgery. Many times this lessens after the surgery although it may take up to two years to improve. Removal or exchange of the lens presently in your eye also may necessitate removal of jelly in the posterior aspect of the eye (vitreous) which can lead to macular edema or injury to the retina (retinal detachment). If you have glaucoma prior to the surgery it is very important to take your medications faithfully. Rarely, drops necessary to help your body accept the transplant make the glaucoma more difficult to control. Proper follow-up with the use of appropriate drops allows us to manage this problem. The success rate for corneal transplant surgery varies depending on the cause of the corneal clouding. Fortunately the most common conditions which require corneal surgery are associated with the highest success rates.
Graft Rejection: Recognizing Signs and Seeking Treatment
An uncommon but important complication of corneal transplantation is graft rejection. Fortunately, the eye is a “privileged site” so unlike other forms of transplantation in the body, corneal transplantation does not require powerful, life threatening medications. Usually drops alone will prevent graft rejection. Graft rejection occurs when the body recognizes the donated cornea as foreign and reacts against it. It happens in approximately 15 % of corneal transplants. The rejection reaction can be treated successfully in 85% of cases, but to do so requires your help. The signs of graft rejection include a red or painful eye, light sensitivity or decreased vision which lasts more than 24 hours. If you note these signs call us immediately and identify yourself as a corneal transplant patient. Arrangements will be made to see you at the soonest possible time. If graft rejection is diagnosed, we will treat with you drops and ointment. The success of treatment of graft rejection increases if we are able to diagnose and treat it early. Thus it is essential that you call us at the first sign of symptoms. We are always happy to see you and will not be upset if we find no sign of graft rejection, but simply alleviate your concern.
Corneal transplantation is performed at the ambulatory surgery center (in and out surgery). Due to the efficiency of the eyebank , it is possible to schedule the transplant. Prior to the surgery you must obtain lab studies and clearance from your medical doctor to be sure that you are fit for surgery. In addition, if an implant will be placed in your eye at the time of surgery , we will require a measurement of the length of your eye. This appointment will be made separately. We will also make arrangements for you to communicate with the anesthesiologist who will help on the day of the surgery.
Almost all corneal surgery is performed under local anesthetic. This includes sedation given by the anesthesiologist to take the edge off the normal nervousness associated with eye surgery, and an injection around the eye to completely numb the eye so you will not feel any pain during the surgery. Local anesthetic is the safest way to perform the surgery and allows the most rapid rehabilitation after surgery. Plan on staying for a total of two to three hours at the surgery center with the operation taking about one to one and one half hours.
Post-Surgery Care and Recovery

After the operation we see you the next day to make sure the transplant looks ok. We will start you on a combination of drops and ointment for the first week . Usually you will be seen twice within the first week, then one week later, two weeks after that and then in one month. You will be using eye drops indefinitely after the surgery, but after the first month you may only need them once per day. We will keep you on a steroid eyedrop to prevent graft rejection. It has no systemic side effects, but can cause progression of a cataract or increase the pressure in your eye, potentially leading to glaucoma, so we must monitor you closely to avoid these side effects. All postoperative care for the first three months is covered by the surgical fee. You should plan on approximately 10 visits within the first year after surgery. If traveling is difficult, I can make arrangements to split the appointments with your local eye doctor. However we always want to remain in contact with you should any problems arise.
We advise you to wear a shield at night for one month to prevent inadvertently rubbing the eye. You can return to your normal activities within a week after surgery, although we caution you not to lift anything that makes you red in the face or to exert yourself excessively for a month after surgery. Also avoid swimming for one month. You can, however, wash your face within the first week and have you hair done, but be careful to keep the eye closed during this time.
Patient-Physician Partnership for Success
I make an agreement with my patients that if you have the surgery, I will take as much time and effort as necessary to make sure that you have a successful outcome. I will try to be available to answer any questions or concerns that you may have about corneal transplantation before or after the operation. In return, it is important that you keep your appointments and are faithful about using the drops. The success of corneal transplantation is a shared responsibility between the patient and the physician.